Burnout among healthcare providers, especially in mental health fields, is a growing concern impacting well-being, patient care, and organizational productivity. Recognizing burnout beyond physical exhaustion, including emotional detachment and reduced personal accomplishment, is crucial. Root causes like heavy workloads, long hours, and lack of control contribute to this issue, with therapy for psychosis cases among the most demanding. Effective prevention strategies involve compassion cultivation practices, mental health education promoting self-care, supportive work environments, and stress management techniques. Integrating therapy for psychosis offers a novel strategy to combat burnout by enhancing resilience, emotional regulation, and understanding of psychotic disorders, ultimately improving patient outcomes and reducing burnout risk.
Healthcare provider burnout is a growing concern, impacting not only individual well-being but also patient outcomes. This article explores comprehensive strategies to prevent burnout among healthcare workers. We delve into understanding the unique challenges they face, from identifying red flags and early warning signs to fostering supportive work environments. Key sections include evidence-based interventions for mental well-being and an innovative focus on integrating therapy for psychosis as a proactive burnout prevention measure.
- Understanding Burnout Among Healthcare Providers
- Identifying Red Flags and Early Warning Signs
- Creating a Supportive Work Environment
- Evidence-Based Interventions for Mental Well-being
- Integrating Therapy for Psychosis in Burnout Prevention
Understanding Burnout Among Healthcare Providers

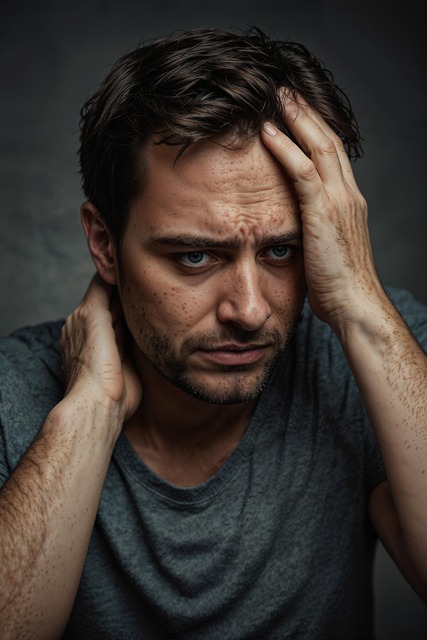
Burnout among healthcare providers is a growing concern, impacting not only individual well-being but also patient care and organizational productivity. It’s essential to recognize that burnout isn’t just physical exhaustion; it encompasses emotional detachment and depersonalization from work, along with feelings of cynicism and reduced personal accomplishment. This phenomenon is particularly prevalent in fields like mental health, where providers frequently deal with high-stress situations and complex cases, such as those involving psychosis.
Understanding the root causes is crucial for developing effective prevention strategies. Many factors contribute to healthcare provider burnout, including heavy workloads, long hours, emotional demands, lack of control over work processes, and insufficient rewards. Incorporating compassion cultivation practices, designing mental health education programs that promote self-care, and fostering supportive work environments can help mitigate these issues. Such approaches not only enhance providers’ resilience but also improve patient outcomes by ensuring a consistent level of care.
Identifying Red Flags and Early Warning Signs

Healthcare providers often face intense workloads and high-stress environments, which can lead to burnout if left unaddressed. Identifying red flags and early warning signs is a crucial step in preventing this issue. Professionals should be vigilant about changes in their emotional state, such as increased irritability, cynicism, or detachment from patients. These symptoms could indicate growing fatigue and disengagement, requiring prompt intervention.
Additionally, observing patterns in professional performance can help recognize burnout. Declines in productivity, frequent errors, or a lack of focus during therapy sessions for psychosis (or other conditions) might suggest that the provider is struggling. Accessing Trauma Support Services and enrolling in Mental Health Education Programs Design can offer valuable tools for managing stress. Incorporating practices like Mindfulness Meditation into daily routines has also proven effective in enhancing resilience and preventing burnout among healthcare professionals.
Creating a Supportive Work Environment

Creating a supportive work environment is a vital strategy to combat burnout among healthcare providers, especially those offering therapy for psychosis. It involves cultivating a culture where empathy and understanding thrive. By implementing empathy building strategies, healthcare workers can feel appreciated and connected to their patients’ journeys, reducing the emotional toll of their demanding roles. This environment should also prioritize open communication and accessibility of resources like trauma support services to address any personal or professional challenges staff may face.
A positive work setting further incorporates effective stress management techniques. Healthcare providers should have access to tools and programs that help them navigate the high-pressure nature of their jobs, ensuring they can deliver quality care without burning out. Regular team meetings, mindfulness workshops, and flexible work arrangements are some ways to foster a supportive atmosphere, ultimately enhancing job satisfaction and well-being.
Evidence-Based Interventions for Mental Well-being

Healthcare providers, like all individuals, are susceptible to mental health challenges, particularly burnout and stress-related disorders. To mitigate these risks, evidence-based interventions for mental well-being have gained prominence in professional healthcare settings. One such intervention is therapy for psychosis, which has shown significant effectiveness in managing symptoms and improving quality of life for affected professionals. Early identification and risk assessment for mental health professionals play a crucial role in preventing severe outcomes.
Community outreach program implementation and trauma support services are also valuable tools. These programs offer a safe space for healthcare providers to discuss their experiences, receive peer support, and access specialized therapy options. By integrating these evidence-based strategies, healthcare organizations can foster a culture of resilience and well-being, ensuring that professionals remain motivated, engaged, and capable of providing quality patient care.
Integrating Therapy for Psychosis in Burnout Prevention

In the context of healthcare provider burnout prevention, integrating therapy for psychosis offers a unique and valuable approach to enhancing resilience and well-being. Beyond addressing mental health challenges, this form of therapy contributes significantly to developing inner strength and fostering mental health awareness among practitioners. By delving into techniques tailored to manage psychotic symptoms, healthcare workers gain tools to navigate stressful situations with enhanced emotional regulation and cognitive flexibility.
Moreover, therapy for psychosis facilitates empathy building strategies that are essential in patient care. Understanding the complexities of psychotic disorders allows healthcare providers to approach patients with greater compassion and nuanced understanding. This not only reduces their own burnout risk but also improves patient outcomes by fostering a supportive and effective therapeutic environment. Through these means, integrating such therapy plays a pivotal role in revolutionizing burnout prevention within the healthcare sector.
Healthcare provider burnout is a complex issue, but by understanding its signs and implementing targeted strategies, it can be effectively prevented. Creating a supportive work environment, utilizing evidence-based interventions for mental well-being, and integrating therapy for psychosis are key components in combating this growing concern. By prioritizing these measures, healthcare organizations can foster a more sustainable and fulfilling workplace, ultimately enhancing patient care and provider satisfaction.